Understanding Shoulder Arthritis: What Every Patient Should Know
Shoulder Arthritis is a degenerative joint condition where protective cartilage breaks down, causing pain, stiffness, and limited mobility. The five main types include osteoarthritis, rheumatoid arthritis, post-traumatic arthritis, rotator cuff tear arthropathy, and avascular necrosis. Symptoms typically worsen over time and include persistent pain, grinding sensations, and sleep disruption.
Treatment ranges from conservative approaches like physical therapy and medications to surgical intervention such as shoulder replacement. Proper post-surgical positioning during sleep is critical for optimal recovery. Most patients can manage symptoms and maintain active lifestyles with appropriate treatment and support.
What Is Shoulder Arthritis?
You’ve been waking up with shoulder pain. Maybe you can’t lift your arm to brush your hair anymore, or reaching for that coffee mug on the top shelf has become impossible. If this sounds familiar, you might be dealing with shoulder arthritis. Shoulder arthritis happens when the smooth cartilage covering your shoulder bones gradually wears away.
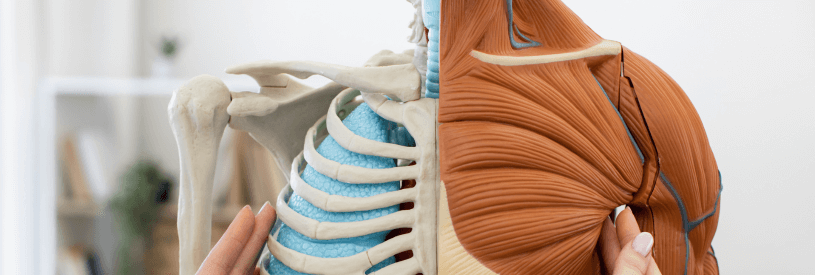
Think of cartilage as the cushioning layer that lets your bones glide smoothly against each other. When it breaks down, bones start rubbing together. That’s when pain, stiffness, and grinding sensations begin. After treating patients with shoulder problems for years, I’ve learned that understanding your condition is the first step toward feeling better. So let’s talk about what’s really happening in your shoulder and what you can do about it.
Your shoulder isn’t just one joint – it’s actually two. The glenohumeral joint is where your upper arm bone (humerus) meets your shoulder blade (scapula). This is the ball-and-socket joint that gives your shoulder its impressive range of motion. The acromioclavicular joint sits at the top of your shoulder where your collarbone meets your shoulder blade. Shoulder arthritis can affect either joint or both. The shoulder is the third most common joint affected by arthritis, after the hip and knee. Unlike your knees, your shoulders don’t bear weight all day. But that doesn’t mean arthritis hurts any less. In fact, shoulder arthritis can be just as disabling because you use your arms for nearly everything.
Types of Shoulder Arthritis
Osteoarthritis
This is the “wear and tear” type. Over time, the cartilage in your shoulder joint simply wears down. It’s like tires on a car – eventually, the tread disappears. Osteoarthritis typically affects people over 50, though younger folks can develop it if they’ve had shoulder injuries or use their shoulders heavily for work or sports. The cartilage gets soft first, then cracks appear, and finally it flakes away. In the end stage, there’s no cushion left. Bone rubs directly on bone.
Rheumatoid Arthritis
Unlike osteoarthritis, rheumatoid arthritis is an autoimmune disease. Your immune system mistakenly attacks the lining of your joint, causing inflammation and pain. This type tends to affect both shoulders equally. What makes rheumatoid arthritis different is that it’s a whole-body condition. If you have it, you’ll likely notice symptoms in other joints too. The good news? Medical treatments for rheumatoid arthritis have improved dramatically in recent years.
Post-Traumatic Arthritis
Did you fracture your shoulder years ago? Dislocate it playing sports? Any injury that damages the cartilage surface can lead to arthritis down the road. Sometimes it develops months after the injury. Sometimes it takes years. I’ve seen patients who had shoulder injuries in their 20s develop arthritis in their 40s or 50s. The initial trauma sets the stage, and normal wear and tear does the rest.
Rotator Cuff Tear Arthropathy
This type develops when you have a large rotator cuff tear that goes untreated. Your rotator cuff is made up of four tendons that hold your shoulder in place and help it move. When these tendons tear completely, the ball of your shoulder (humeral head) can shift upward and rub against other bones. Over time, this abnormal movement damages the cartilage. Only about 4% of people with rotator cuff tears develop this type of arthritis. But when it happens, it’s particularly challenging to treat because both the soft tissue and joint surface are damaged.
Avascular Necrosis
This is the least common type but one of the most serious. Avascular necrosis means “bone death from lack of blood supply.” When blood flow to the ball of your shoulder gets interrupted, the bone tissue dies. As the dead bone collapses, it damages the cartilage covering it. What causes this? High-dose steroid use, heavy alcohol consumption, sickle cell disease, or traumatic injuries. Sometimes we can’t identify a cause at all.
Recognizing the Symptoms
Pain
Pain is usually the first sign. At first, you’ll only hurt during activity. Reaching overhead, lifting objects, or throwing a ball triggers the discomfort. But as arthritis progresses, pain shows up even at rest. Many of my patients tell me the pain sits deep in the shoulder. It might radiate down your arm to the elbow. Some days are worse than others, and changes in weather can make it flare up.
Night pain is particularly common. You’ll shift positions all night trying to get comfortable, but nothing works. This sleep disruption becomes one of the most disabling aspects of shoulder arthritis.
Stiffness and Limited Motion
You might notice you can’t reach as far behind your back. Putting on a jacket becomes awkward. Washing your hair requires creative maneuvering. This loss of motion usually creeps up gradually. You compensate without realizing it until one day you notice you can’t do something that used to be automatic.
Grinding, Clicking, and Popping
When cartilage wears away, the joint surfaces become rough and irregular. As your shoulder moves, you might hear or feel grinding (doctors call this crepitus). Sometimes it’s loud enough for others to hear. These noises don’t always hurt, but they’re a sign that cartilage damage is present. Some patients describe a catching or locking sensation.
Weakness
As arthritis progresses, your shoulder can feel weak. This isn’t always true muscle weakness. Often it’s your body’s protective response to pain. You unconsciously limit how much force you apply because movement hurts.
How Shoulder Arthritis Is Diagnosed
Physical Examination
When you come to my office with shoulder pain, I’ll check several things. I’ll test your range of motion, both when you move your arm yourself and when I move it for you. I’ll feel for tender spots and check your strength. One key finding with arthritis is that both active and passive motion hurt. If only active motion (when you move it yourself) hurts, that suggests a different problem, like a rotator cuff tear without arthritis.
Imaging Tests
X-rays are the gold standard for diagnosing shoulder arthritis. They show the space between your bones. In a healthy shoulder, you’ll see a gap where cartilage cushions the joint. As arthritis progresses, that space narrows. In severe cases, bone touches bone with no space at all.
- X-rays also reveal bone spurs (osteophytes). These are bony growths that develop around arthritic joints. They’re your body’s attempt to stabilize the joint, but they often make stiffness worse.
- CT scans provide more detailed bone images. Your doctor might order one if surgery is being considered.
- MRI scans excel at showing soft tissues. They’re particularly useful for checking your rotator cuff tendons and determining if you have rotator cuff tear arthropathy.
Diagnostic Injections
Sometimes we’re not sure if shoulder pain is coming from arthritis or another source. A diagnostic injection of local anesthetic (with or without cortisone) can help. If your pain disappears after the injection, even temporarily, arthritis is likely the culprit.
Treatment Options: What Works
Non-Surgical Approaches
Most patients start here, and many find enough relief that they don’t need surgery.
Activity Modification
You don’t have to stop using your arm, but you might need to change how you use it. If lifting heavy objects triggers pain, reduce the weight. If overhead activities hurt, minimize them when possible. I tell patients to let pain be their guide. Some discomfort during activity is normal, but if pain lasts hours afterward or wakes you at night, you’ve done too much.
Ice and Heat
Ice reduces inflammation and numbs pain. Apply it for 20-30 minutes several times daily, especially after activities that aggravate your shoulder. Always use a barrier between ice and skin to prevent frostbite. Heat can loosen stiff joints before activity. A warm shower or heating pad helps many patients with morning stiffness.
Physical Therapy
A good physical therapist can teach you exercises to maintain or improve your range of motion. Gentle stretching prevents your shoulder from getting even stiffer. Strengthening exercises help stabilize your shoulder, but they need to be carefully chosen. The wrong exercises can make arthritis pain worse.
Medications
Over-the-counter options include acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen. NSAIDs reduce both pain and inflammation, but they can irritate your stomach. Take them with food, and talk to your doctor if you have a history of ulcers or kidney problems. Prescription medications may offer stronger relief or fewer side effects. Your doctor can discuss options based on your overall health.
Cortisone Injections
Injecting cortisone directly into your shoulder joint can dramatically reduce inflammation and pain. The effect varies—some patients get months of relief, others just weeks. You can’t get injections indefinitely because repeated cortisone can weaken tissues. If you’re considering shoulder replacement surgery, avoid cortisone injections for at least three months beforehand. They can increase infection risk after surgery.
Shoulder Arthritis Surgical Treatment: From Arthroscopy to Replacement
When non-surgical treatments stop working and pain significantly limits your life, surgery might be your best option.
Arthroscopic Debridement
For mild to moderate arthritis, a surgeon can use an arthroscope (a small camera) to “clean out” your joint. This involves removing loose cartilage fragments, smoothing rough areas, and cleaning up inflammation. This procedure doesn’t cure arthritis, but it can relieve pain for 12-24 months, sometimes longer. It’s less invasive than joint replacement and has a quicker recovery.
Shoulder Replacement
For advanced arthritis, shoulder replacement is highly effective. The surgeon removes damaged bone and cartilage, replacing them with metal and plastic components. Total shoulder replacement replaces both the ball (humeral head) and socket (glenoid). It’s the standard option for most types of shoulder arthritis.
Reverse total shoulder replacement switches the normal anatomy—the ball goes on the socket side and the socket on the humeral side. This design works well for rotator cuff tear arthropathy because it relies on your deltoid muscle instead of your damaged rotator cuff. Shoulder replacements typically last 15-20 years or more. Most patients experience dramatic pain relief and improved function.
When to See Your Doctor
Don’t wait until you can barely move your arm. Early evaluation means more treatment options.
See your doctor if:
- Shoulder pain persists for more than a few weeks
- Pain interferes with daily activities or sleep
- You notice progressive loss of motion
- Over-the-counter medications aren’t helping
- Your shoulder feels unstable or gives way
If you’ve already been diagnosed with shoulder arthritis, check in with your doctor if symptoms worsen despite treatment or if you develop new symptoms.
Living with Shoulder Arthritis
Protecting Your Shoulder
Small changes can make a big difference. Use your non-affected arm for heavy lifting when possible. Organize your home so frequently used items are easy to reach. Consider assistive devices like a long-handled shoehorn or grabber tool. At work, evaluate your workspace. Can you adjust your chair height or monitor position to reduce shoulder strain? Talk to your employer about modifications if your job requires repetitive shoulder use.
Staying Active
You might be tempted to stop exercising altogether, but that’s usually counterproductive. Your shoulder needs movement to maintain flexibility. The key is choosing the right activities. Swimming and water aerobics are excellent because water supports your arm’s weight. Walking, cycling, and elliptical machines keep you fit without stressing your shoulder. Yoga can help with flexibility, but avoid poses that put weight on your arms.
The Critical Role of Sleep
Here’s something many patients don’t realize: sleep quality directly affects your recovery and pain levels. Your body repairs damaged tissues during deep sleep. Poor sleep increases inflammation and makes pain feel worse. Shoulder arthritis makes sleep particularly challenging. You can’t lie on the affected side, and finding a comfortable position becomes increasingly difficult. Many patients resort to sleeping in a recliner, but this creates its own problems. Recliners rarely provide quality sleep, and most people only manage about two hours before waking in pain.
Proper positioning during sleep is especially critical after shoulder surgery. Your shoulder needs to be supported in what orthopedic surgeons call the “maximally loose packed position“—a specific angle that minimizes stress on healing tissues while reducing swelling.
Recovery After Shoulder Surgery
If you’re facing shoulder surgery, preparing for recovery is just as important as the surgery itself. You’ll need help with daily activities for several weeks. Stock up on groceries, prepare meals you can freeze, and set up a recovery space with everything within easy reach. Post-surgical positioning is critical. Your surgeon will give you specific instructions about how to position your arm. Following these guidelines precisely can mean the difference between a smooth recovery and complications.
The Restore You Therapeutic Support system by Surgical Recovery Systems addresses one of the most challenging aspects of shoulder surgery recovery: getting quality sleep in the proper healing position. This FDA-registered, medical-grade device is specifically engineered to maintain your shoulder and chest in the optimal position throughout the night. Unlike generic pillows or sleeping in a recliner, the Restore You enables 6-8 hours of uninterrupted, restorative sleep by supporting your entire torso and both arms in the precise position your shoulder needs for healing. Clinical data shows it helps reduce post-surgical opioid use by 50% while patients report a 96% satisfaction rate. The device is made in the USA with patented technology designed by medical professionals who understand that proper sleep positioning isn’t just about comfort—it’s about accelerating your healing and getting you back to the activities you love.
Final Thoughts
Shoulder arthritis can be frustrating and painful, but you’re not without options. From simple lifestyle modifications to surgical intervention, treatments exist that can help you manage symptoms and maintain an active life. The key is staying proactive. Don’t ignore persistent shoulder pain. Work with your healthcare provider to develop a treatment plan that fits your lifestyle and goals. And remember that recovery—whether from arthritis or surgery—takes time and patience. If you’re dealing with shoulder arthritis or facing shoulder surgery, reach out to an orthopedic specialist. They can evaluate your specific situation and recommend the best path forward for your unique needs.
Medical Disclaimer: This article provides general information about shoulder arthritis and should not replace professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment recommendations specific to your condition. Individual results may vary based on overall health, age, and the severity of arthritis.